
The POS plans usually have lower premiums because they offer fewer options.ĭo you have to choose a PCP with a PPO or POS? Typically you will have a higher premium with a PPO because it offers more options. Premiums: This is what you pay monthly for your plan.With a POS plan coinsurance costs could kick in if you need out-of-network care or fail to get referrals to see other providers. For a PPO plan your coinsurance kicks in once you've met your deductible. Coinsurance: You may be required to share some of the costs for your care with both a PPO and POS plan.

This is a fee you pay to a doctor at the time of a visit or for a prescription medication.

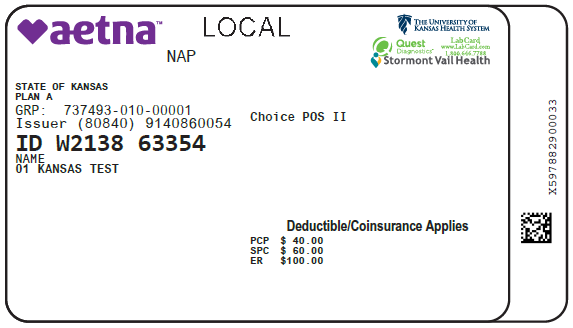
POS plans typically do not have a deductible as long as you choose a Primary Care Provider, or PCP, within your plan's network and get referrals to other providers, if needed. This means you pay for care and services until the deductible is met. Deductibles: PPO plans usually come with a deductible.Primary Care Provider (PCP) requirement.Costs ( deductibles, coinsurance, copays, and premiums).Here are some main features that you can compare to find out what makes a PPO different from a POS: This way you can make a decision based on your needs. When you're comparing health plans it's important to understand what sets them apart from one another. PPO vs POS: What are the main differences? There are many more details you'll want to compare, as well. POS, or Point of Service plans, have lower costs, but with fewer choices. A PPO, or Preferred Provider Organization, offers a lot of flexibility to see the doctors you want, at a higher cost. Urgent Care (benefit availability may vary by location)Ĭopay waived if admitted deductible waived.Ĭovered 80% after deductible for emergency use 60% after deductible for non-emergency useĬovered 100% emergency use 60% non-emergency use after deductibleĬovered 80% after deductible and $250 per admission copay.Ĭopay applies only to first 2 hospital stays per year.Ĭovered 60% after $500 per admission copay.Ĭovered 80% after deductible and $250 per admission copayĬovered 80% after $100 outpatient surgery facility copay deductible waived (excluding surgery)Ĭost sharing applies to all covered benefits incurred during any inpatient stay or outpatient visitġ00% after $40 copay deductible waived (benefits based on place of service)Ĭovers diagnosis and treatment of underlying cause only.In general the biggest difference between PPO vs. Routine Digital Rectal Exam/Prostate-specific Antigen Test Routine Adult Physical Exams/ Immunizationsġ exam per 12 months for members age 18 and older.ġ7 exams in the first 12 months of life 3Įxams in the 2nd 12 months of life 3 exams in 3rd 12 months 1 exam per Included services of an internist, general physician, family practitioner, or pediatrician for routine care, as well as diagnosis and treatment of an illness or injury.ġ00% per visit no copay or deductible appliesġ00% after $25 PCP or $40 specialist office visit copay deductible waivedġ If performed as part of a physician office visit and billed by physician, expenses are covered subject to the applicable physician's office visit member cost sharing. Primary Care Physician Office Visit (non-surgical) Once family payment limit is met, all family members will be considered as having met their payment limit for the remainder of the calendar year. Note: if enrolled in the High Deductible Consumer Plan with dependent(s), the family deductible will apply and must be met prior to benefits being payable unless otherwise indicated.ĢOnly those out-of-pocket expenses resulting from the application of coinsurance percentage and deductibles (except any penalty amounts) may be used to satisfy the payment limit.ģCoinsurance, copays and deductibles count towards payment limits. All covered expenses cross-apply toward both the in and out-of-network deductibles. Once the family deductible is met, all family members will be considered as having met their deductible for the remainder of the year. Certification for hospital admissions, treatment facility admissions, skilled nursing facility admissions, home health care, hospice care is required – excluded amount applied separately to each type of expense is $200 per occurrence.ġUnless otherwise indicated the deductible must be met prior to benefits being payable. Making Benefits Changes During the YearĬertification for certain types of out-of-network care must be obtained to avoid a reduction in benefits paid for that care.Enhanced Maternity Short-Term Disability and Parental Leave.Leaves of Absence & Disability Insurance.Health ConnectionSM Disease Management Program.


 0 kommentar(er)
0 kommentar(er)
